Written by Manal Usmani and Edited by Catherine Zhang
Medical device companies create products to combat specific diseases and illnesses. One such product, the artificial heart valve, has helped tackle the debilitating effects of structural heart disease in millions of patients. This type of cardiovascular disease involves the malfunction of the heart valves, which are structures of the heart that allow blood to flow in the right direction through the heart and out to the organs in the body. When the valves become weak and do not close completely, blood does not flow in the right direction [1]. Consequently, a disruption occurs in the distribution of oxygenated blood to the organs and deoxygenated blood to the lungs [2]. Since the heart is the organ that takes oxygen from the lungs and delivers it to the rest of the body, structural issues can result in insufficient oxygenated blood delivery to vital organs such as the brain. Because of this, artificial heart valves can be life-saving and life-changing for patients.
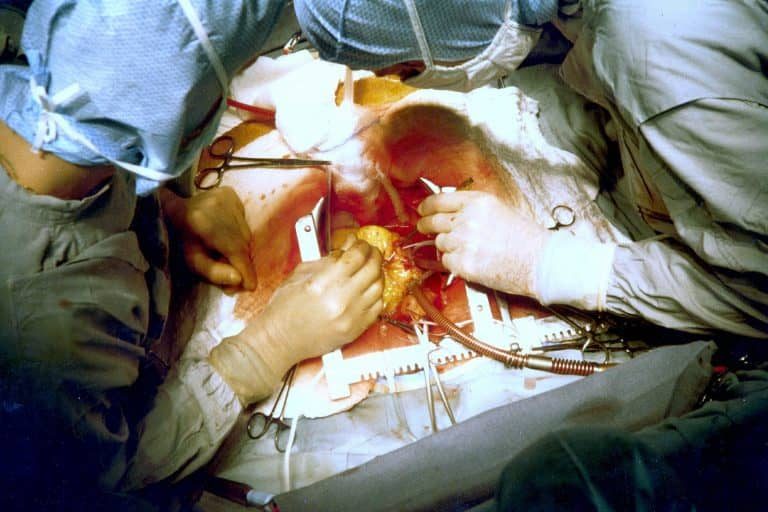
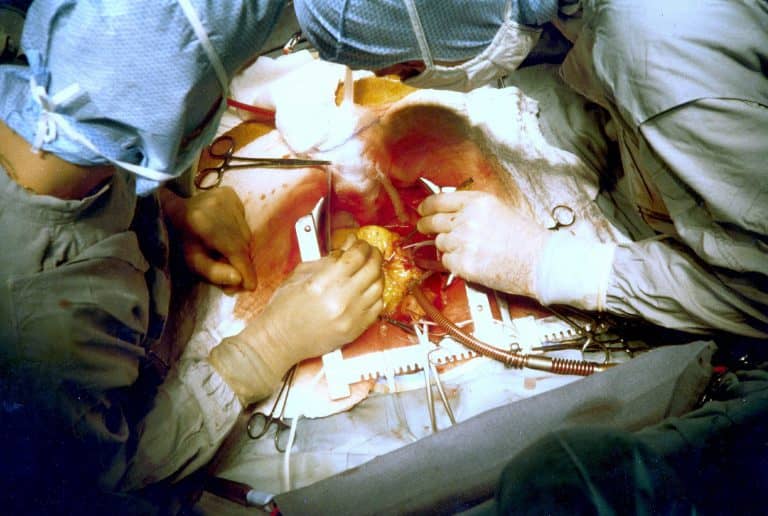
Previous methods of inserting artificial heart valves involved cracking open the chest and stopping the heart during surgery [3]. In the present, however, non-invasive approaches that do not require breaking the ribs to access the heart have been developed. This novel procedure called ‘transcatheter heart valve replacement’ decreases both the postoperative recovery time and the complications associated with putting the heart on bypass when it is stopped [4].
Currently, the valves that have had success in replacement procedures include: the aortic valve, which opens to allow oxygenated blood to flow to the organs; the mitral valve, which allows oxygenated blood to be loaded into the heart; and the tricuspid valve, which allows deoxygenated blood to reach the lungs. All of these valves have to close at certain times in the cardiac cycle to prevent backflow and allow sufficient oxygen delivery to the organs [5].
Data from clinical trials using transcatheter valves have shown a 98.4% decrease in mortality rates and a 97% decrease in valve malfunction three years after implantation [6]. These promising results demonstrate that most patients experience a restorative effect in which the heart returns to normal functioning. Implications for these results are that artificial heart valves allow patients to have a better quality of life and an evidence-supported avenue for preventative measures against structural heart disease.
With every invasive procedure, however, it is important to keep in mind that there are always some associated risks involved. Patients considering artificial valve replacement should know that there might be complications due to the slight chance of manufacturing errors of the valves or due to the unique biology of every individual receiving the new valve. Furthermore, while the cost of the transcatheter valve replacement procedure is comparable to surgical valve replacement, the supplies can be more expensive for the non-invasive procedure [7]. As a result, it is essential to perform a cost-benefit analysis with your physician before committing to this revolutionary procedure because every patient is unique and their full background needs to be taken into consideration prior to the treatment.
References:
- Jaffer, I.H., Whitlock, R.P. (2016). A mechanical heart valve is the best choice. Heart Asia, 8:4-62.
- Maganti, K, Rigolin, V.H., Sarano, M.E., Bonow, R.O. (2010). Valvular heart disease: diagnosis and management. Mayo Clinic proceedings, 85:483-500.
- Berg, S. K., Zwisler, A, Pederson, B.D. (2013). Patient experiences of recovery after heart valve replacement: suffering weakness, struggling to resume normality. BMC nursing, 12:100-123.
- Baumbach, Hardy et al. (2019). Transcatheter aortic valve replacement- management of patients with significant coronary artery disease undergoing aortic valve interventions: surgical compared to catheter-based approaches in hybrid procedures. BMC cardiovascular disorders, 19:100-108.
- Sacks, M.S., Yoganathan, A.P. (2007). Heart valve function: a biomechanical perspective. Philosophical transactions of the Royal Society of London, 362:1369-1391.
- Kenny, D, Rhodes, J.F., Fleming, G.A. (2018). 3-Year Outcomes of the Edwards SAPIEN Transcatheter Heart Valve for Conduit Failure in the Pulmonary Position From the COMPASSION Multicenter Clinical Trial. JACC: Cardiovascular interventions, 11:1920-1929.
- Meduri, C, Chung, J, Gaffney, J, Henley, S, Williams, J, Gada, H. (2017). TCT-787 Comparison of U.S. Hospital Costs Between Transcatheter Aortic Valve Replacement (TAVR) and Surgical Aortic Valve Replacement (SAVR). JACC: Cardiovascular interventions, 70:1016-1040.